Sep 29
Sepsis
Sepsis
World Sepsis Day on September 13 serves as an annual reminder of a global health crisis, but for those of us on the front lines of aged care, the fight against sepsis is a daily reality. Sepsis is not a distant threat; it is one of the most common causes of death worldwide, responsible for an estimated 11 million deaths in a single year, which accounts for a staggering 20% of all global deaths. It is a condition that demands our constant vigilance, deep understanding, and swift, decisive action. This is especially true in aged care facilities, where we care for one of the most vulnerable populations.
What Exactly is Sepsis?
It is crucial to understand that sepsis is not the infection itself. Instead, sepsis is a life-threatening medical emergency that occurs when the body has an extreme and unregulated response to an infection. An infection from any source—whether it's a urinary tract infection, pneumonia, a skin wound, an abdominal infection or from another source, such as dental, minor injuries or surgical procedure—can trigger this devastating chain reaction.
Instead of fighting the infection locally, the body’s immune system overreacts, triggering a large, widespread inflammatory response. This systemic reaction, intended to protect, ultimately damages the body’s own tissues and organs. Without prompt treatment, this can quickly cause tissue damage, multiple organ failure, septic shock, and death.
Instead of fighting the infection locally, the body’s immune system overreacts, triggering a large, widespread inflammatory response. This systemic reaction, intended to protect, ultimately damages the body’s own tissues and organs. Without prompt treatment, this can quickly cause tissue damage, multiple organ failure, septic shock, and death.
Why is Aged Care a High-Risk Environment?
While anyone can develop sepsis from any infection, residents in our care are at a markedly higher risk. Most individuals who develop sepsis have at least one underlying medical condition, which is common in aged care. The specific risk factors that come together in our facilities include:
- Older Age: Individuals aged 65 and over are a primary at-risk group.
- Weakened immune systems: The natural aging process can reduce the immune response, making it more difficult for the body to combat initial infections.
- Chronic Medical Conditions: Pre-existing illnesses such as diabetes, lung disease, cancer, or kidney disease weaken the body's resilience and increase susceptibility.
- Indwelling Medical Devices: Catheters, enteral feeding tubes, and other devices can serve as entry points for bacteria, increasing the risk of infection.
- Recent Hospitalisation or Surgery: Many of our residents may have had recent hospital stays, which is a recognised risk factor for developing sepsis.
- Poor Nutrition or Hydration: These factors can further weaken the body's ability to combat an infection.

Recognising Sepsis: Sepsis can be deceptive in the elderly.
One of the biggest challenges in aged care is that sepsis can be incredibly deceptive. Its initial presentation is often subtle and may be mistaken for normal signs of aging or a simple infection. Importantly, typical infection symptoms like fever are often missing in older people. This requires us to stay alert and watch for any sudden, unexplained changes in a resident’s condition.
From Subtle to Severe: The Progression of Sepsis
Understanding the stages of sepsis is key to appreciating the need for speed.
- Early, Milder Presentation (Sepsis): In the initial stage, the body is initiating its inflammatory response, but significant organ damage has not yet taken place. This is our prime opportunity for intervention. Signs are often non-specific and may include a new or worsening fever, an abnormally low body temperature, rapid heart rate, quick breathing, or chills. Sudden and unexplained confusion or disorientation is a critical red flag in the elderly.
- Severe Sepsis:The infection and inflammation have become severe enough to affect organ function. Symptoms of sepsis are present, along with signs of organ dysfunction – such as difficulty breathing, abnormal liver tests or reduced urine output.
- Progressive, Severe Presentation (Septic Shock): If sepsis is not treated promptly, the inflammatory response worsens, causing septic shock. This is the critical stage at which organs begin to fail rapidly. Symptoms become much more serious and noticeable: extremely low blood pressure, mottled or discoloured skin, little to no urine, severe breathlessness, and possible loss of consciousness. The chance of survival drops significantly at this stage.
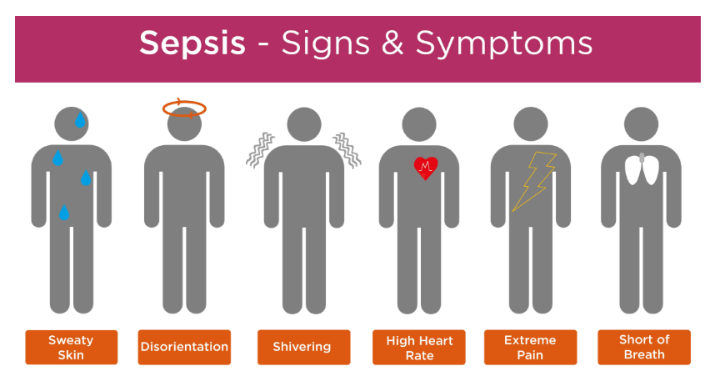
Know the Signs and Symptoms
It's important to look for a cluster of symptoms. While you don't need to have all of them, the presence of several should raise concern.
Common general signs and symptoms include:
- Fever, shivering, or feeling very cold
- Confusion, disorientation, or slurred speech
- High heart rate, weak pulse, or low blood pressure
- Rapid or difficult breathing (shortness of breath)
- Extreme body pain, discomfort, or muscle pain
- Clammy or sweaty skin
- Feeling very tired or lethargic
- Low urine output (passing no urine in a day)
A simple way to remember some key signs is the SEPSIS acronym:
- Slurred speech or confusion
- Extreme shivering or muscle pain
- Passing no urine (in a day)
- Severe breathlessness
- It feels like you’re about to die (a resident might say they're feeling the worst ever).
- Skin that appears mottled or discoloured
If you observe any sudden, unexplained change in a resident's condition—such as worsening dementia, extreme lethargy, unresponsiveness, or an unexplained fall—treat it as though it could be sepsis. If a resident with a known infection declines further, always ask yourself: ‘Could it be sepsis?’
From Suspicion to Action: The Critical First Hour and the "Sepsis Six"
When it comes to sepsis, every moment counts. Early diagnosis and prompt, appropriate clinical management are vital to increasing survival chances. Treatment is most effective when initiated as soon as possible.
The foundation of rapid intervention is the "Sepsis Six" bundle—a set of six essential actions that should be carried out within the first hour of recognising suspected sepsis. These steps are a priority for every healthcare professional.
The foundation of rapid intervention is the "Sepsis Six" bundle—a set of six essential actions that should be carried out within the first hour of recognising suspected sepsis. These steps are a priority for every healthcare professional.
1. Provide Oxygen: Administer high-flow oxygen to maintain target saturation levels and support organ function.
2. Take Blood Cultures: Prior to administering antibiotics, collect blood cultures to identify the specific pathogen responsible for the infection.
3. Administer broad-spectrum antibiotics immediately: Do not wait for culture results. Use intravenous broad-spectrum antibiotics to quickly combat the most probable bacterial causes.
4. Administer Intravenous Fluids: Initiate fluid resuscitation using intravenous fluids to support blood pressure and ensure proper perfusion to vital organs.
5. Measure Blood Lactate: A blood lactate level is a vital indicator of organ dysfunction and the severity of sepsis.
6. Measure Urine Output: Accurately monitor and record urine output to assess kidney function, which is often one of the first organs to be affected.
2. Take Blood Cultures: Prior to administering antibiotics, collect blood cultures to identify the specific pathogen responsible for the infection.
3. Administer broad-spectrum antibiotics immediately: Do not wait for culture results. Use intravenous broad-spectrum antibiotics to quickly combat the most probable bacterial causes.
4. Administer Intravenous Fluids: Initiate fluid resuscitation using intravenous fluids to support blood pressure and ensure proper perfusion to vital organs.
5. Measure Blood Lactate: A blood lactate level is a vital indicator of organ dysfunction and the severity of sepsis.
6. Measure Urine Output: Accurately monitor and record urine output to assess kidney function, which is often one of the first organs to be affected.
The Role of Antimicrobials and the Challenge of Resistance
Antimicrobials, especially antibiotics, are essential for treating infections that can lead to sepsis. However, the rise of antimicrobial resistance (AMR) presents a major challenge. Sepsis acquired in healthcare environments is often caused by drug-resistant pathogens, which can cause a swift deterioration in a patient's health. Patients with resistant pathogens have a greater risk of dying in hospitals.
This highlights the significance of two key principles:
This highlights the significance of two key principles:
- Rapid Administration: When sepsis is suspected, antibiotics should be administered promptly.
- Antibiotic Stewardship: We must also act as responsible stewards of these vital drugs. This involves using them only when needed, making sure residents finish prescribed courses, and avoiding unnecessary use to prevent the development of resistance.
Prevention: Our First and Best Line of Defence
The most effective way to prevent sepsis is to stop infections before they start. As healthcare workers in aged care, we have a strong ability to lower the risk of sepsis through careful and proactive care. Key prevention strategies include:
- Meticulous Infection Control: This is non-negotiable. It includes strict adherence to hand hygiene, the use of aseptic techniques for all procedures, and thorough cleaning of equipment and the environment.

- Promoting Vaccinations: Ensure residents are up to date with recommended vaccinations, such as for influenza and pneumonia, to prevent common infections that can lead to sepsis.
- Proper Wound Care: Keep all cuts and wounds clean and covered until they are fully healed to prevent skin infections.
- Managing Chronic Illnesses: Collaborate with the broader healthcare team to ensure residents' chronic conditions, such as diabetes or lung disease, are well-controlled, as this enhances their overall resistance to infection.
- Proactive Screening and Monitoring: Utilise structured screening tools such as the National Early Warning Score (NEWS) or Modified Early Warning Score (MEWS) to regularly monitor residents, particularly those with new or worsening infections.
- Staff Education: Ongoing training for all staff on the signs and symptoms of sepsis and the importance of prompt reporting is essential to fostering a culture of safety
Beyond Survival: The Ongoing Effects of Post-Sepsis Syndrome
For those who survive, the battle might not end there. Many residents can experience long-lasting physical, psychological, and emotional effects known as post-sepsis syndrome. This can persist for months and may include symptoms like severe muscle and joint pain, extreme fatigue, difficulty sleeping, nightmares, panic attacks, trouble concentrating, and loss of confidence. Awareness of this syndrome is essential for providing comprehensive, long-term support to our residents' post-sepsis.
A Shared Global Mission
The work you do each day in your facility contributes to a global effort. Combating sepsis is recognised by the World Health Organisation (WHO) as a global health priority and is crucial for meeting Sustainable Development Goals related to lowering maternal and child mortality and improving the quality of care. Your dedication directly supports this worldwide mission.
A Shared Global Mission
The work you do each day in your facility contributes to a global effort. Combating sepsis is recognised by the World Health Organisation (WHO) as a global health priority and is crucial for meeting Sustainable Development Goals related to lowering maternal and child mortality and improving the quality of care. Your dedication directly supports this worldwide mission.
Conclusion: You Are the Key
Sepsis is a formidable adversary, especially in aged care settings. Its subtle onset in older adults requires a high level of clinical suspicion and vigilance from every member of the care team. Recognising the subtle signs is the first and most vital step in a swift, coordinated response that can save lives.
By implementing practices such as routine screening, maintaining strict infection control, and being ready to activate the "Sepsis Six" bundle at a moment's notice, we can significantly enhance outcomes for our residents. Remember, with sepsis, every minute counts. Your proactive care, keen observational skills, and prompt action are the most powerful tools we have in the fight against this silent killer.
By implementing practices such as routine screening, maintaining strict infection control, and being ready to activate the "Sepsis Six" bundle at a moment's notice, we can significantly enhance outcomes for our residents. Remember, with sepsis, every minute counts. Your proactive care, keen observational skills, and prompt action are the most powerful tools we have in the fight against this silent killer.
Sepsis: A message from the IPS Team
World Sepsis Day 2025 – Tools to Support Your Sepsis Protocols
On September 13, we join the global health community in commemorating World Sepsis Day, a vital reminder of the urgent need to raise awareness, prevent, and respond to this life-threatening condition.
This year’s campaign, led by the Global Sepsis Alliance, emphasises “5 Facts x 5 Actions”. It highlights five key messages about the global impact of sepsis and five steps that every health system and facility can take to save lives.
On September 13, we join the global health community in commemorating World Sepsis Day, a vital reminder of the urgent need to raise awareness, prevent, and respond to this life-threatening condition.
This year’s campaign, led by the Global Sepsis Alliance, emphasises “5 Facts x 5 Actions”. It highlights five key messages about the global impact of sepsis and five steps that every health system and facility can take to save lives.
5 Facts About Sepsis
Sepsis is the leading cause of death worldwide, claiming a life every 3 seconds.
It disproportionately impacts the most vulnerable. Children, the elderly, and immunocompromised individuals are at greatest risk.
Most deaths from sepsis can be prevented with infection control and early detection.
Despite its significance, only a small number of countries have established sepsis policies.
An enhanced sepsis response is essential to achieving global health and pandemic preparedness targets.
Sepsis is the leading cause of death worldwide, claiming a life every 3 seconds.
It disproportionately impacts the most vulnerable. Children, the elderly, and immunocompromised individuals are at greatest risk.
Most deaths from sepsis can be prevented with infection control and early detection.
Despite its significance, only a small number of countries have established sepsis policies.
An enhanced sepsis response is essential to achieving global health and pandemic preparedness targets.
5 Actions to Strengthen the Sepsis Response
Call for prioritising and funding sepsis response efforts at both national and local levels.
Develop sepsis protocols and ensure staff are appropriately trained.
Support research, innovation, and sharing resources.
Raise awareness of this urgent emergency.
Embed sepsis prevention and treatment into pandemic and emergency response plans
Call for prioritising and funding sepsis response efforts at both national and local levels.
Develop sepsis protocols and ensure staff are appropriately trained.
Support research, innovation, and sharing resources.
Raise awareness of this urgent emergency.
Embed sepsis prevention and treatment into pandemic and emergency response plans
Your Facility Challenge
We challenge all facilities to review and discuss their current sepsis procedures and protocols with their teams. Consider:
Are staff confident in recognising the early signs of sepsis?
Do you have clear escalation and communication pathways in place?
Is your sepsis response in line with the latest guidelines?
To support this, we are providing two practical IPS tools:
The IPS Sepsis Flowchart – a clear decision-support guide for screening and escalation.
The IPS SBAR Tool for Sepsis – a structured communication method to ensure accurate and consistent handover.
By dedicating time to World Sepsis Day to raise awareness and refine protocols, we can work together to reduce preventable deaths and improve patient outcomes across all care settings.
Thank you for your ongoing commitment to patient safety.
Warm regards,
Dianne, Senior Clinical Consultant, IPS
We challenge all facilities to review and discuss their current sepsis procedures and protocols with their teams. Consider:
Are staff confident in recognising the early signs of sepsis?
Do you have clear escalation and communication pathways in place?
Is your sepsis response in line with the latest guidelines?
To support this, we are providing two practical IPS tools:
The IPS Sepsis Flowchart – a clear decision-support guide for screening and escalation.
The IPS SBAR Tool for Sepsis – a structured communication method to ensure accurate and consistent handover.
By dedicating time to World Sepsis Day to raise awareness and refine protocols, we can work together to reduce preventable deaths and improve patient outcomes across all care settings.
Thank you for your ongoing commitment to patient safety.
Warm regards,
Dianne, Senior Clinical Consultant, IPS

How would your facility cope with a case of sepsis? Have this information readily available to care teams and incorporate it into training scenarios. Prevent a case of sepsis before it happens!
Further information can be obtained from the HUB or EVE. If you would rather, contact our friendly team at support@infectionprevention.care
We are on Facebook and LinkedIn. Like, follow and share to those you know.
Take advantage of our expertise in IPC. See the HUB for policies, resources and courses relating to this very important subject. Ask EVE for a quick answer to your question.
Further information can be obtained from the HUB or EVE. If you would rather, contact our friendly team at support@infectionprevention.care
We are on Facebook and LinkedIn. Like, follow and share to those you know.
Take advantage of our expertise in IPC. See the HUB for policies, resources and courses relating to this very important subject. Ask EVE for a quick answer to your question.
Lyndon Forrest
Managing Director | CEO
I am a passionate and visionary leader who has been working in the field of infection prevention and control in aged care for almost 30 years. I am one of the co-founders and the current Managing Director and CEO of Bug Control New Zealand and Australia, the premium provider of infection prevention and control services in aged care. I lead a team that is driven by a common purpose: to help aged care leaders and staff protect their residents from infections and create a healthier future for them.
I am building a business that focuses on our clients and solving their problems. We are focused on building a world-class service in aged care. We focus on being better, not bigger, which means anything we do is for our clients.
I am a passionate and visionary leader who has been working in the field of infection prevention and control in aged care for almost 30 years. I am one of the co-founders and the current Managing Director and CEO of Bug Control New Zealand and Australia, the premium provider of infection prevention and control services in aged care. I lead a team that is driven by a common purpose: to help aged care leaders and staff protect their residents from infections and create a healthier future for them.
I am building a business that focuses on our clients and solving their problems. We are focused on building a world-class service in aged care. We focus on being better, not bigger, which means anything we do is for our clients.
Erica Callaghan
Marketing Manager
Erica Callaghan is a dedicated professional with a rich background in agriculture and nutrient management. Growing up on her family's farm in Mid Canterbury, she developed a deep passion for farming. She currently resides on her partner's arable property in South Canterbury.
In 2017, Erica joined the Farm Sustainability team, focusing on nutrient management and environmental stewardship. In February 2024, she became the Manager of Marketing and Sales at Bug Control New Zealand - Infection Prevention Services, where her passion now includes improving infection prevention outcomes.
Outside of work, Erica loves cooking and traveling, often combining her culinary interests with her explorations in Italy and Vietnam. She enjoys entertaining family and friends and remains actively involved in farm activities, especially during harvest season.
Erica Callaghan is a dedicated professional with a rich background in agriculture and nutrient management. Growing up on her family's farm in Mid Canterbury, she developed a deep passion for farming. She currently resides on her partner's arable property in South Canterbury.
In 2017, Erica joined the Farm Sustainability team, focusing on nutrient management and environmental stewardship. In February 2024, she became the Manager of Marketing and Sales at Bug Control New Zealand - Infection Prevention Services, where her passion now includes improving infection prevention outcomes.
Outside of work, Erica loves cooking and traveling, often combining her culinary interests with her explorations in Italy and Vietnam. She enjoys entertaining family and friends and remains actively involved in farm activities, especially during harvest season.
Toni Sherriff
Clinical Nurse Specialist
Toni is a Registered Nurse with extensive experience in Infection Prevention and Control. Her career began as a kitchen hand and caregiver in Aged Care facilities, followed by earning a Bachelor of Nursing.
Toni has significant experience, having worked in Brisbane’s Infectious Diseases ward before returning home to New Zealand, where she continued her career as a Clinical Nurse Specialist in Infection Prevention and Control within Te Whatu Ora (Health NZ).
Toni brings her expertise and dedication to our team, which is instrumental in providing top-tier infection prevention solutions to our clients.
Toni is a Registered Nurse with extensive experience in Infection Prevention and Control. Her career began as a kitchen hand and caregiver in Aged Care facilities, followed by earning a Bachelor of Nursing.
Toni has significant experience, having worked in Brisbane’s Infectious Diseases ward before returning home to New Zealand, where she continued her career as a Clinical Nurse Specialist in Infection Prevention and Control within Te Whatu Ora (Health NZ).
Toni brings her expertise and dedication to our team, which is instrumental in providing top-tier infection prevention solutions to our clients.
Julie Hadfield
Accounts & Payroll
Julie is experienced in Accounts & Payroll Administration & after a long career in both the Financial & Local Government Sectors, is now working with our team. Julie brings her strong time management & organisational skills to our team, which is important to keep the company running in the background to enable the rest of our team to provide top notch service to all of our clients.
Julie is experienced in Accounts & Payroll Administration & after a long career in both the Financial & Local Government Sectors, is now working with our team. Julie brings her strong time management & organisational skills to our team, which is important to keep the company running in the background to enable the rest of our team to provide top notch service to all of our clients.
Andrea Murray
Content Editor
I attended Otago University in NZ and graduated as a Dental Surgeon. After 40 years in the profession, I retired in 2022. Infection prevention knowledge was part of everyday practice, dealing with sterilisation, hand hygiene, and cleaning.
Before retiring, I began doing some editing and proofreading for Bug Control as I am interested in the subject and in the English language. During the COVID-19 lockdown, I attended the ACIPC course "Introduction to Infection Prevention and Control", which increased my interest in the subject. I now work part-time as the Content Editor for the company.
I attended Otago University in NZ and graduated as a Dental Surgeon. After 40 years in the profession, I retired in 2022. Infection prevention knowledge was part of everyday practice, dealing with sterilisation, hand hygiene, and cleaning.
Before retiring, I began doing some editing and proofreading for Bug Control as I am interested in the subject and in the English language. During the COVID-19 lockdown, I attended the ACIPC course "Introduction to Infection Prevention and Control", which increased my interest in the subject. I now work part-time as the Content Editor for the company.
Personally, I lived in the UK for 10 years. My two children were born in Scotland, and now both are living in Europe, one in Amsterdam, Netherlands, and the other in Edinburgh, Scotland. I live close to Fairlie on the South Island of NZ, a beautiful part of the country, and I love being out of the city.
Princess
Customer Support
Princess began her career as a dedicated Customer Service Representative, honing her communication and problem-solving skills. She later transitioned into a Literary Specialist role, where she developed a keen eye for detail. Her journey then led her to a Sales Specialist position, where she excelled in client relations.
Now, as a Customer Support professional in Infection Prevention Services. Princess focuses on ensuring customer satisfaction, building loyalty, and enhancing the overall customer journey.
Princess began her career as a dedicated Customer Service Representative, honing her communication and problem-solving skills. She later transitioned into a Literary Specialist role, where she developed a keen eye for detail. Her journey then led her to a Sales Specialist position, where she excelled in client relations.
Now, as a Customer Support professional in Infection Prevention Services. Princess focuses on ensuring customer satisfaction, building loyalty, and enhancing the overall customer journey.
Dianne Newey
Senior Infection Prevention and Control Consultant
With over 35 years of experience as a Registered Nurse, I'm now applying all my experience and skills as a Senior Infection Prevention and Control Consultant with Bug Control Infection Prevention Advisory Services.
This is through IP&C education, IP&C environmental audits and reports, IP&C policy and procedure review and development and consultancy on infection prevention and control issues. When I’m not working, I spend time with my family and in my garden, where I grow all my own veggies.
With over 35 years of experience as a Registered Nurse, I'm now applying all my experience and skills as a Senior Infection Prevention and Control Consultant with Bug Control Infection Prevention Advisory Services.
In my role, I promote Infection Prevention and Control, to RACF's and disability support services.
This is through IP&C education, IP&C environmental audits and reports, IP&C policy and procedure review and development and consultancy on infection prevention and control issues. When I’m not working, I spend time with my family and in my garden, where I grow all my own veggies.
Caoimhe (Keva) Stewart
Clinical & Business Operations Manager
Caoimhe is the Manager of Customer Service at Bug Control | Infection Prevention Services, where she ensures that learners have a seamless and supportive experience. With her previous experience as a Registered Nurse in both the UK and Australia, Caoimhe brings a deep understanding of healthcare to her role. Before joining Bug Control IPS Services, she worked in a variety of nursing settings, including Occupational Health, Palliative Care, and Community Nursing, providing her with the ability to empathise with learners and understand the challenges they face.
Caoimhe is the Manager of Customer Service at Bug Control | Infection Prevention Services, where she ensures that learners have a seamless and supportive experience. With her previous experience as a Registered Nurse in both the UK and Australia, Caoimhe brings a deep understanding of healthcare to her role. Before joining Bug Control IPS Services, she worked in a variety of nursing settings, including Occupational Health, Palliative Care, and Community Nursing, providing her with the ability to empathise with learners and understand the challenges they face.
Her move from nursing to customer service was driven by her passion for helping others, not just in clinical settings but also in ensuring that people have access to the resources and support they need. Now, Caoimhe applies her problem-solving skills, attention to detail, and communication expertise to her role, helping to create a positive and effective learning environment for all students.
Outside of work, Caoimhe enjoys travelling, staying active, and catching up with friends on the weekends. Whether in healthcare or customer service, she’s dedicated to making a meaningful difference and supporting people in their personal and professional growth.
Bridgette Mackie
Clinical Nurse Educator
Bridgette is an experienced New Zealand Registered Nurse, qualified Healthcare Auditor, and Healthcare Educator with a strong background in clinical quality, competency assessment, and infection prevention. She has led large-scale OSCE and CAP training programmes for internationally qualified nurses, developed sector-specific educational resources, and coordinated HealthCERT audit preparation in the surgical sector.
Known for her engaging teaching style and genuine passion for supporting learners, Bridgette excels at making complex topics accessible and relevant. She blends operational leadership with a deep commitment to professional development and safe, effective practice.
Bridgette is an experienced New Zealand Registered Nurse, qualified Healthcare Auditor, and Healthcare Educator with a strong background in clinical quality, competency assessment, and infection prevention. She has led large-scale OSCE and CAP training programmes for internationally qualified nurses, developed sector-specific educational resources, and coordinated HealthCERT audit preparation in the surgical sector.
Known for her engaging teaching style and genuine passion for supporting learners, Bridgette excels at making complex topics accessible and relevant. She blends operational leadership with a deep commitment to professional development and safe, effective practice.

