The Dawn of Modern Infection Control
- Ignaz Semmelweis: A Pioneer of Infection Control

In this era, women were attending hospitals more often to give birth in a seemingly safer environment than the more traditional birth at home with a midwife. Maternity institutions often provided care to underprivileged women, who then became subjects for the training of doctors and midwives as a method of payment. The rising infection and death rates began to soar, and the maternity institutions tried to address the reasons behind this rise. The miasma theory was the understanding, at that time, of the cause of infection, where illness arose from “bad air” emanating from decaying organic matter.
Amidst these dilemmas, Ignaz Semmelweis, a Hungarian
physician, embarked on a journey that would revolutionise infection control. In
1846, he took the role of assistant at the First Obstetrical Clinic of the
Vienna General Hospital. It was there that he observed an unsettling disparity
in maternal mortality rates. The First Clinic, staffed by doctors and medical
students, recorded a significantly higher mortality rate from infection,
averaging around 10%, compared to the Second Clinic, where only midwives were
trained, which reported rates below 4%. This substantial difference ignited
Semmelweis's curiosity, and he embarked on a meticulous investigation into the
underlying causes. Through careful observation and analysis, Semmelweis ruled
out various potential factors, including overcrowding, climate, and even
religious practices. Similar medical techniques were noted as common to both
clinics. The consistent divergence in mortality rates, despite comparable
conditions and procedures, indicated that a unique element associated with the involvement of medical students in the First Clinic was the case. This conclusion highlighted the power of observational studies in identifying disease aetiologies.
The tragic death in 1847 of Semmelweis's esteemed friend and colleague, Professor Jakob Kolletschka, was a pivotal moment. Kolletschka died from an infection after an accidental puncture from the scalpel of a student during a post-mortem examination. The autopsy findings from Kolletschka were strangely the same as those of the women who had died from puerperal fever. This similarity led Semmelweis to a groundbreaking deduction: he theorised that he and the medical students performing autopsies were inadvertently transmitting "cadaverous particles" from the autopsy room to the patients in the First Obstetrical Clinic during examinations. In contrast, the midwives in the Second Clinic did not perform autopsies and had no contact with corpses. The direct correlation Semmelweis identified between Kolletschka's death from contamination following autopsy and the symptoms of puerperal fever represented a decisive piece of reasoning, leading him to his revolutionary hypothesis regarding disease transmission.

Semmelweis's groundbreaking work occurred before the acceptance of the germ theory of disease. While he correctly identified the transmission of "cadaverous particles" as causative agents in the deaths from puerperal fever, he lacked the understanding of the microorganisms responsible. It was the subsequent work of Louis Pasteur and others studying germ theory that provided the scientific foundation for Semmelweis's observations, confirming that microorganisms were indeed the causative agents of diseases like puerperal fever. The "morbid poison" that Semmelweis suspected was being transmitted was likely the bacteria known as Group A haemolytic streptococcus. Despite his lack of knowledge about the specific microorganisms, Semmelweis's implementation of washing hands with chlorinated lime proved effective because this solution possessed powerful antibacterial properties. Semmelweis's findings, despite an incomplete theoretical framework at the time, were remarkably accurate and ushered in the acceptance of germ theory in the understanding and prevention of infectious diseases.
Despite the compelling evidence from his work, Semmelweis faced significant criticism and rejection from the established medical community. His findings challenged the medical opinions of the day, including the widely held miasma theory and the belief that each case of disease was unique. Many doctors were deeply offended by the implication that they were responsible for the deaths of their patients. Furthermore, Semmelweis struggled to clearly express an explanation for his findings that was accepted by his contemporaries. His personality and often confrontational communication style further aggravated the resistance he encountered. The phenomenon known as the "Semmelweis reflex" aptly describes the tendency to reject new evidence simply because it contradicts established beliefs or norms. The resistance Semmelweis faced showed the potent influence of existing theories in science and the difficulties in accepting revolutionary ideas, even when supported by strong evidence. The concept of the "Semmelweis reflex" remains a reminder of the challenges faced in embracing new medical knowledge.
Despite these setbacks in Vienna, Semmelweis continued his efforts in Budapest, where he achieved similar success in dramatically reducing the incidence of childbed fever. He eventually published his seminal work, "The Aetiology, Concept, and Prophylaxis of Childbed Fever," in 1861, but it initially failed to be widely accepted. Tragically, Semmelweis's mental health deteriorated, and he died in an asylum in 1865. It was only years after his death, with the acceptance of germ theory in medicine, that his profound contributions were finally recognised. Today, Ignaz Semmelweis is rightfully celebrated as the "saviour of mothers" and a true pioneer in the field of infection control.
2.The Genesis of Medical Gloves
In the field of surgical practice, the latter part of the 19th century marked a crucial transition with the introduction of medical gloves. Before this innovation, surgeons and physicians typically attended to patients with their bare hands. Surgery in this era was essentially a death sentence, with mortality rates around 50% in the late 1800s, and post-operative infections a leading cause of these dire outcomes. Basic hygiene practices, including the simple act of handwashing between surgical procedures, were not consistently followed. The high incidence of post-operative infections in the preglove era accentuated the urgent need for effective barrier methods to prevent the transmission of pathogenic microorganisms during surgical procedures.
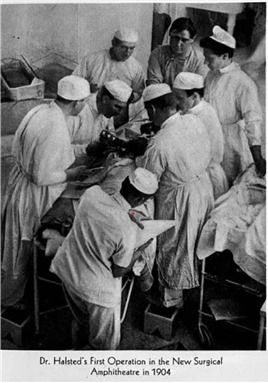
The introduction of surgical
gloves is widely attributed to Dr. William Halsted, a prominent surgeon at
Johns Hopkins Hospital in Baltimore, USA. However, the initial impetus behind
the innovation of gloves was not primarily focused on preventing infection in
patients. In 1889, Dr. Halsted introduced rubber gloves to protect his scrub
nurse, Caroline Hampton, from the severe contact dermatitis she developed due
to prolonged exposure to the harsh chemical disinfectants, such as mercuric
chloride and carbolic acid, which were used for sterilisation. To assist her
with the dermatitis, Halsted commissioned the Goodyear Rubber Company to produce
custom-made thin rubber gloves with gauntlets. Caroline Hampton, also his
fiancée, first donned these rubber gloves in 1889 (See illustration above). The
gloves proved to be a successful solution, leading to the provision of
additional pairs for the surgeons and other members of the operating theatre staff.
By June 1890, the use of surgical gloves had become a common practice in many
hospitals. The swift adoption of gloves by surgical teams, initially motivated
by personal protection, inadvertently produced a more aseptic surgical
environment, leading ultimately to the recognition of their role in reducing
infections in surgical patients.
Early Medical Glove Materials and Manufacturing:
The first surgical gloves were crafted from thin rubber,
most likely natural latex, produced by the Goodyear Rubber Company. They were
described as "thin with gauntlets". These early gloves were not
intended for single use; instead, they were sterilised between surgical
procedures, and reused. Sterilisation methods involved boiling the gloves or
using chemical agents like carbolic acid. The reliance on reusable rubber
gloves provided an early challenge to maintain a consistently sterile surgical
environment, as the effectiveness of sterilisation could vary.
A significant advancement in rubber technology came in 1839,
with Charles Goodyear's discovery of vulcanisation. This process, which
involved treating crude rubber with sulphur and heat, resulted in a stronger,
more durable, and less plastic material. Vulcanised rubber quickly became the
preferred material for protective medical gloves. Goodyear's innovation was
pivotal in making rubber a reliable material for medical applications, enabling
it to become an effective barrier rather than a substance susceptible to
temperature changes.
Before the advent of rubber gloves, basic forms of hand protection were used in medicine. Historical records show that as early as 1758, an obstetrician named Walbaum used rudimentary gloves made from sheep intestine. Other physicians employed gloves made of cotton, silk, or leather. However, these earlier forms of hand protection were often too bulky and lacked the tactile sensitivity and dexterity of the later rubber gloves. The use of materials like sheep intestine suggests an early awareness of the need for hand protection in medical settings, even before a full and comprehensive understanding of infection transmission.
Advantages of Early Medical Gloves
The introduction of these early medical gloves brought several key advantages to healthcare practices. Initially, their primary benefit was protecting healthcare workers from the harsh chemical irritants used for disinfection. By creating a physical barrier, these gloves prevented direct contact with disinfectant substances like carbolic acid and mercuric chloride, which caused severe dermatitis. While initially some surgeons believed that gloves would hinder their dexterity, others soon realised that the rubber material could improve their grip on surgical instruments, especially when hands were wet or slippery. The introduction of gloves represented a vital step towards establishing barrier precautions in medical settings. Although the understanding of germ theory was yet to be fully accepted, the introduction of gloves was a significant step towards recognising the importance of preventing direct contact with blood and body fluids. Perhaps most importantly, the use of gloves, in conjunction with the principles of antiseptic surgery, contributed to a significant reduction in post-operative infection rates. The observations made by surgeons like Joseph Bloodgood, who had an obvious decline in infections during hernia operations with the use of gloves, provided the crucial evidence for their effectiveness. This reduction in infection rates helped reinforce the role of medical gloves in surgical practice.
Disadvantages and Limitations of Early Medical Gloves
Despite their emerging benefits, early medical gloves also
presented several limitations. One significant issue was the development of
skin irritation and latex allergies among healthcare workers. The prolonged use
of rubber gloves, especially in a moist environment created by perspiration,
often leads to skin irritations. Furthermore, as the use of latex gloves became
more widespread, latex allergies emerged as a significant occupational concern
for those in healthcare, necessitating the development of alternative glove
materials. Initially, some surgeons resisted the adoption of gloves, fearing
diminished tactile sensation in delicate surgical procedures. This resistance
highlighted the tension between the growing awareness of infection control and
the practical demands of surgical techniques.
Early medical gloves were also reused, and while sterilisation methods like boiling and carbolic acid were employed, their effectiveness may not have been consistently reliable, leading to cases of cross-contamination between patients. The later introduction of disposable gloves would address this critical limitation. Furthermore, the early rubber gloves were more susceptible to tearing or punctures, compromising their effectiveness as a barrier. This problem highlighted the need for improvements in material strength and manufacturing quality. Finally, the lack of a complete understanding of germ theory initially hindered the full appreciation of the benefits of gloves in preventing infection, with the primary focus still on protecting the wearer from chemical irritants.
The Impact of Scientific Advancements on Glove Adoption
The widespread acceptance of the germ theory of disease, from the work of Louis Pasteur and others, provided the scientific rationale for the importance of hand hygiene and barrier protection to prevent infections. Joseph Lister's pioneering work on antiseptic surgery further emphasised the prevention of microbial contamination during surgical procedures. These advancements provided the scientific understanding that promoted the importance of medical gloves in preventing the spread of infection. The mid-20th century witnessed a significant evolution towards sterile and disposable gloves, enhancing safety and convenience further in medical practice. Furthermore, to address the growing issue of latex allergies, the development of alternative glove materials such as nitrile and vinyl provided options for healthcare professionals and patients. These materials offered varying degrees of protection, durability, and tactile sensitivity, catering to specific medical needs.

Conclusion
Take advantage of our expertise in IPC. See the HUB for policies, resources and courses relating to this very important subject. Ask EVE for a quick answer to your question.
Lyndon Forrest
I am a passionate and visionary leader who has been working in the field of infection prevention and control in aged care for almost 30 years. I am one of the co-founders and the current Managing Director and CEO of Bug Control New Zealand and Australia, the premium provider of infection prevention and control services in aged care. I lead a team that is driven by a common purpose: to help aged care leaders and staff protect their residents from infections and create a healthier future for them.
I am building a business that focuses on our clients and solving their problems. We are focused on building a world-class service in aged care. We focus on being better, not bigger, which means anything we do is for our clients.
Erica Callaghan
Erica Callaghan is a dedicated professional with a rich background in agriculture and nutrient management. Growing up on her family's farm in Mid Canterbury, she developed a deep passion for farming. She currently resides on her partner's arable property in South Canterbury.
In 2017, Erica joined the Farm Sustainability team, focusing on nutrient management and environmental stewardship. In February 2024, she became the Manager of Marketing and Sales at Bug Control New Zealand - Infection Prevention Services, where her passion now includes improving infection prevention outcomes.
Outside of work, Erica loves cooking and traveling, often combining her culinary interests with her explorations in Italy and Vietnam. She enjoys entertaining family and friends and remains actively involved in farm activities, especially during harvest season.
Toni Sherriff
Toni is a Registered Nurse with extensive experience in Infection Prevention and Control. Her career began as a kitchen hand and caregiver in Aged Care facilities, followed by earning a Bachelor of Nursing.
Toni has significant experience, having worked in Brisbane’s Infectious Diseases ward before returning home to New Zealand, where she continued her career as a Clinical Nurse Specialist in Infection Prevention and Control within Te Whatu Ora (Health NZ).
Toni brings her expertise and dedication to our team, which is instrumental in providing top-tier infection prevention solutions to our clients.
Julie Hadfield
Julie is experienced in Accounts & Payroll Administration & after a long career in both the Financial & Local Government Sectors, is now working with our team. Julie brings her strong time management & organisational skills to our team, which is important to keep the company running in the background to enable the rest of our team to provide top notch service to all of our clients.
Andrea Murray
I attended Otago University in NZ and graduated as a Dental Surgeon. After 40 years in the profession, I retired in 2022. Infection prevention knowledge was part of everyday practice, dealing with sterilisation, hand hygiene, and cleaning.
Before retiring, I began doing some editing and proofreading for Bug Control as I am interested in the subject and in the English language. During the COVID-19 lockdown, I attended the ACIPC course "Introduction to Infection Prevention and Control", which increased my interest in the subject. I now work part-time as the Content Editor for the company.
Princess
Princess began her career as a dedicated Customer Service Representative, honing her communication and problem-solving skills. She later transitioned into a Literary Specialist role, where she developed a keen eye for detail. Her journey then led her to a Sales Specialist position, where she excelled in client relations.
Now, as a Customer Support professional in Infection Prevention Services. Princess focuses on ensuring customer satisfaction, building loyalty, and enhancing the overall customer journey.
Dianne Newey
With over 35 years of experience as a Registered Nurse, I'm now applying all my experience and skills as a Senior Infection Prevention and Control Consultant with Bug Control Infection Prevention Advisory Services.
This is through IP&C education, IP&C environmental audits and reports, IP&C policy and procedure review and development and consultancy on infection prevention and control issues. When I’m not working, I spend time with my family and in my garden, where I grow all my own veggies.
Caoimhe (Keva) Stewart
Caoimhe is the Manager of Customer Service at Bug Control | Infection Prevention Services, where she ensures that learners have a seamless and supportive experience. With her previous experience as a Registered Nurse in both the UK and Australia, Caoimhe brings a deep understanding of healthcare to her role. Before joining Bug Control IPS Services, she worked in a variety of nursing settings, including Occupational Health, Palliative Care, and Community Nursing, providing her with the ability to empathise with learners and understand the challenges they face.
Bridgette Mackie
Bridgette is an experienced New Zealand Registered Nurse, qualified Healthcare Auditor, and Healthcare Educator with a strong background in clinical quality, competency assessment, and infection prevention. She has led large-scale OSCE and CAP training programmes for internationally qualified nurses, developed sector-specific educational resources, and coordinated HealthCERT audit preparation in the surgical sector.
Known for her engaging teaching style and genuine passion for supporting learners, Bridgette excels at making complex topics accessible and relevant. She blends operational leadership with a deep commitment to professional development and safe, effective practice.

