Sep 20
Understanding and Overcoming Burnout & Compassion Fatigue in Aged Care
In the heart of Australia’s and New Zealand's aged care facilities, nurses and caregivers play a role that is both deeply rewarding and incredibly demanding. They are the pillars of support for our residents, providing not just physical care but also emotional comfort, companionship, and dignity. However, this dedication often comes at a cost, leading to two challenging yet often misunderstood conditions: staff burnout and compassion fatigue. These are not merely signs of weakness but signals that the immense pressures of your vital work are taking a significant toll.

This blog post aims to shed light on these "invisible epidemics," helping you understand what they are, how they differ, why they happen, and most importantly, what both individuals and organisations can do to prevent and deal with them. Your well-being is vital, not just for you, but for the quality of care you provide with passion
What is Burnout?
Burnout is much more than just feeling tired after a long shift; it's a deep sense of exhaustion that can develop gradually over time. The World Health Organisation (WHO) describes it as a syndrome caused by ongoing workplace stress that hasn't been
properly managed. It's not a medical condition on its own, but an occupational phenomenon that significantly affects your professional life.
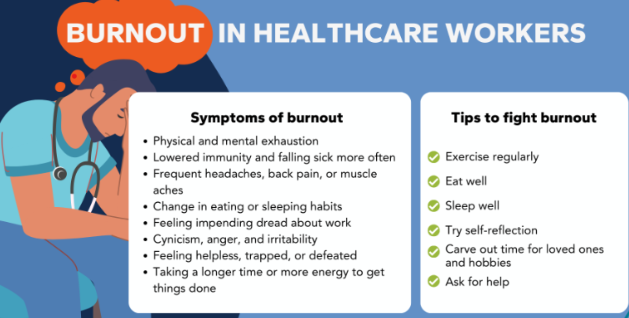
Burnout typically manifests through three key components:
Burnout typically manifests through three key components:
- Emotional Exhaustion: This is a feeling of being depleted, drained of energy, and utterly worn out. You might feel like you have nothing left to give, both emotionally and physically.
- Cynicism and Detachment: You might notice yourself developing a negative, callous, or distant attitude towards your work, your workplace, and even the people you care for. This can feel like a growing sense of cynicism about your job or responsibilities.
- Reduced Professional Efficacy: This refers to a marked decline in your sense of personal achievement and competence, causing you to feel that your efforts are futile. You might experience a lack of accomplishment despite working hard.

Common signs and symptoms of burnout include severe physical and emotional exhaustion, feeling increasingly detached from your responsibilities, reduced productivity, and a lack of motivation or interest. While burnout can affect anyone in any profession, it is particularly widespread in high-pressure environments like aged care. Research by Dr. Raechel Damarell has identified a high prevalence of burnout in the residential and home care workforce in countries like Australia, ranging from 30-50%.
What Exactly Is Compassion Fatigue?
Often confused with burnout, compassion fatigue is a distinct condition, also known as secondary trauma or vicarious trauma. It is the state of physical, mental, or emotional exhaustion that occurs when you experience prolonged exposure to someone else’s suffering. This condition is closely linked to the deep empathy and care you give to people in distress.
Compassion fatigue is extremely common among those in caring professions, including family caregivers, nurses, doctors, and home health aides. It emerges when your "well of compassion has been drained dry" from the continuous demand for empathy. As Dr. Eric Zillmer, Professor of Neuropsychology, explains, "Compassion is a meta-cognitive process… You can't live there. It would be cognitively exhausting."
Compassion fatigue is extremely common among those in caring professions, including family caregivers, nurses, doctors, and home health aides. It emerges when your "well of compassion has been drained dry" from the continuous demand for empathy. As Dr. Eric Zillmer, Professor of Neuropsychology, explains, "Compassion is a meta-cognitive process… You can't live there. It would be cognitively exhausting."
Common symptoms and signs of compassion fatigue include:
- Feeling hopeless and experiencing a decreased ability to empathise, often described as emotional numbness. You may struggle to feel compassion towards those in your care.
- A sense of detachment from your surroundings or from people in need.
- Anxiety and irritability.
- Physical symptoms such as headaches, gastrointestinal issues, disrupted sleep, and chronic tiredness.
- Excessive rumination and concern about others' suffering.
- Feelings of sadness, helplessness, or even blaming yourself or others for not doing enough.
Compassion fatigue develops gradually over time, moving through stages from empathetic ability and response to compassion stress, and ultimately to compassion fatigue if the stress is not managed. It is a cumulative process, especially with prolonged, continuous, and intense exposure to stress.
Burnout vs. Compassion Fatigue: The Key Differences
While both conditions involve considerable emotional and physical exhaustion, recognising their unique origins and signs is vital for effective intervention.
1. Origin and Cause:
- Burnout mainly results from ongoing workplace stress that isn't effectively managed. It's associated with high pressure and job exhaustion.
- Compassion fatigue results from prolonged exposure to others' suffering and vicarious trauma. It specifically refers to the emotional toll of caring for those in distress.
2. Emotional Impact:
- Burnout often leads to cynicism and frustration towards your job or workplace, making you feel unappreciated, undervalued, or resentful. It leads to dissatisfaction at work.
- Compassion fatigue causes difficulty empathising, emotional numbness, and a sense of detachment from those in need. You might experience guilt about not being able to care for others as you once did, which can lead to feelings of helplessness and hopelessness.
3. Behavioural Symptoms:
- People experiencing burnout may exhibit procrastination, reduced productivity, increased absence from work, and out-of-character disagreements with colleagues. These symptoms often improve when they are away from work.
- Compassion fatigue can lead to withdrawal from social activities, a loss of interest in things once enjoyed, and sometimes unhealthy coping mechanisms. It may also manifest as secondary traumatic stress symptoms, similar to PTSD, such as nightmares, sleep difficulties, and intrusive thoughts related to the trauma observed.
4.Physical Symptoms:
- Burnout is linked to insomnia, heart palpitations, a weakened immune system leading to frequent illnesses, and can even contribute to serious long-term health problems like heart disease and type 2 diabetes.
- Compassion fatigue often leads to common stress-related physical symptoms such as headaches, fatigue, gastrointestinal problems, and sleep disturbances.
5. Onset and Scope:
Essentially, burnout depletes your professional energy, leaving you exhausted by your job, while compassion fatigue drains your empathic capacity, making you tired from caring for others' suffering.
- Burnout usually develops gradually and is often limited to work responsibilities. It can occur in any profession.
- Compassion fatigue can sometimes occur suddenly and tends to affect overall life satisfaction beyond just work. It is especially common in professions involving direct patient care and exposure to trauma.
Essentially, burnout depletes your professional energy, leaving you exhausted by your job, while compassion fatigue drains your empathic capacity, making you tired from caring for others' suffering.

Why Do We Experience This? Unpacking the Causes
The aged care environment, while deeply rewarding, presents unique challenges that contribute to both burnout and compassion fatigue.
Factors Making Burnout Worse in Aged Care:
Factors Making Burnout Worse in Aged Care:
- Excessive Workloads and Staffing Shortages: This is a persistent problem. Not enough staff and heavy workloads create ongoing time pressure, making it hard to deliver the person-centred care you aim for. This leads to moral distress – the emotional pain of knowing the right action but being unable to take it due to limitations.
- Lack of Resources: Not having access to essential material resources, such as adequate PPE during the COVID-19 crisis, directly affects your ability to perform your role effectively and safely, increasing stress. Providing the necessary resources (time, training, materials) is vital for delivering optimal care.
- Limited Voice and Control: Feeling that you have no say in workplace problem-solving, schedules, or care plans can lead to feelings of helplessness and disempowerment.
- Unacknowledged Grief and Emotional Toll: Aged care workers often build long-term bonds with residents. When a resident passes away, it can cause genuine grief, which is frequently overlooked by colleagues and organisations. Suppressing this grief to seem professional can lead to emotional fatigue, a major factor in burnout.
- Lack of Support and Recognition: Insufficient managerial and peer support, as well as a lack of acknowledgement for your hard work, significantly contribute to burnout. Feeling isolated, undervalued, or even bullied, increases stress levels.
- Inadequate Training: Being unprepared for the demands of your role because of insufficient training can leave you feeling overwhelmed and less confident.
- Systemic issues such as inadequate pay and staffing shortages are major factors, although they are not always quickly fixable by individual facilities.
- Constant Health Risks: The ongoing threat of infectious diseases causes significant anxiety. The fear of contracting or spreading a virus to vulnerable residents weighs heavily on them.
- Stigma and Public Scrutiny: The aged care sector has faced significant public scrutiny, which can cause staff to feel undervalued, blamed, or demoralised.
Factors Contributing to Compassion Fatigue:
- Prolonged Exposure to Suffering: In aged care, workers are continually confronted with residents' decline, illness, and death, many experiencing complex health issues. This ongoing exposure to others' pain is the main cause of compassion fatigue.
- The Demand for Empathy: While empathy is vital, the ongoing and excessive pressure to empathise can be emotionally exhausting.
- Feeling Helpless or Out of Control: When you see suffering but feel powerless to alleviate it completely, or lack control over the situation, your risk of compassion fatigue increases.
- High Stress Levels and Poor Coping Skills: Existing high stress, coupled with limited personal coping strategies or a lack of social support, increases vulnerability to compassion fatigue.
- History of Trauma: Individuals with their own trauma history may be more vulnerable to secondary trauma through their work.
What Individuals Can Do to Cultivate Personal Resilience
Addressing burnout and compassion fatigue requires a multi-faceted approach, involving both individual strategies and strong organisational support. "Telling staff to take care of themselves isn't enough".
You are the most valuable resource in aged care, and protecting your well-being is not a luxury but a necessity.
1. Prioritise Self-Care: This is essential. Ensure you get enough sleep (7-9 hours), eat a balanced diet, and stay active regularly. Make time for hobbies, relaxation, and quality time with loved ones – activities that restore your emotional and physical energy and bring you happiness. Remember, "You can't pour from an empty cup."
2. Set and Enforce Boundaries: It's vital to clearly define your work hours and responsibilities. Master the art of saying "no" to extra demands when you're off the clock and disconnect from work-related messages. This helps create a healthy separation between your professional and personal life. Recognise and accept what you can't control and focus on what you can.
3. Find Your Support Network: Chat with trusted colleagues, friends, or family about your experiences. Sharing your struggles can lessen feelings of isolation and offer new perspectives. Peer support is priceless.
4. Practice Mindfulness: Techniques such as deep breathing, meditation, or even a few minutes of quiet reflection can help manage stress, anxiety, and depression in the moment, building emotional regulation over time.
5. Seek Professional Help: If you're experiencing symptoms of burnout or compassion fatigue, don't hesitate to seek professional support. A therapist or counsellor can provide valuable insights, teach coping strategies, and address any underlying mental health issues. Many workplaces offer Employee Assistance Programs (EAPs) that provide free and confidential counselling.
6. Take Breaks and Manage your Workload: If possible, take mental health days or a few days off to rest and recharge without work pressure. Look for opportunities to adjust your workload, such as reducing your client load or temporarily working in a different area of care.
7. Reassess Priorities: Take a step back and think about what truly matters. Can you delegate tasks, lighten your workload, or discover a new purpose in your work?
8. Engage in Professional Development: Training in stress management, resilience building, and coping strategies can be a lifeline, helping you endure stress and increasing job satisfaction.
You are the most valuable resource in aged care, and protecting your well-being is not a luxury but a necessity.
1. Prioritise Self-Care: This is essential. Ensure you get enough sleep (7-9 hours), eat a balanced diet, and stay active regularly. Make time for hobbies, relaxation, and quality time with loved ones – activities that restore your emotional and physical energy and bring you happiness. Remember, "You can't pour from an empty cup."
2. Set and Enforce Boundaries: It's vital to clearly define your work hours and responsibilities. Master the art of saying "no" to extra demands when you're off the clock and disconnect from work-related messages. This helps create a healthy separation between your professional and personal life. Recognise and accept what you can't control and focus on what you can.
3. Find Your Support Network: Chat with trusted colleagues, friends, or family about your experiences. Sharing your struggles can lessen feelings of isolation and offer new perspectives. Peer support is priceless.
4. Practice Mindfulness: Techniques such as deep breathing, meditation, or even a few minutes of quiet reflection can help manage stress, anxiety, and depression in the moment, building emotional regulation over time.
5. Seek Professional Help: If you're experiencing symptoms of burnout or compassion fatigue, don't hesitate to seek professional support. A therapist or counsellor can provide valuable insights, teach coping strategies, and address any underlying mental health issues. Many workplaces offer Employee Assistance Programs (EAPs) that provide free and confidential counselling.
6. Take Breaks and Manage your Workload: If possible, take mental health days or a few days off to rest and recharge without work pressure. Look for opportunities to adjust your workload, such as reducing your client load or temporarily working in a different area of care.
7. Reassess Priorities: Take a step back and think about what truly matters. Can you delegate tasks, lighten your workload, or discover a new purpose in your work?
8. Engage in Professional Development: Training in stress management, resilience building, and coping strategies can be a lifeline, helping you endure stress and increasing job satisfaction.

What Organisations Can Do: Fostering a Supportive Environment
Organisations play a vital role in establishing a workplace culture that prevents and reduces burnout and compassion fatigue.
1. Acknowledge and Support Grief: Recognising that staff develop long-term relationships with residents, organisations must offer bereavement support when residents pass away. This recognises the compassionate end-of-life care given and values the emotional investment of workers.
2. Foster a Supportive Workplace Culture: Beyond individual efforts, organisations can greatly reduce burnout by creating a culture where staff feel genuinely supported. This involves tackling issues such as feelings of isolation, being undervalued, or bullying.
3. Create Psychologically Safe Spaces: Actively foster environments and opportunities for staff to share their experiences, concerns, and stresses without fear of judgment.
4. Provide Adequate Resources and Training: Ensure staff have the necessary material resources, time, and regular training programs to deliver the best possible care. Opportunities for career advancement also boost job satisfaction and preparedness.
5. Recognise and Appreciate Efforts: Staff who feel their contributions are valued and acknowledged as "making a difference" are less likely to experience burnout. Celebrate their efforts regularly.
6. Empower Staff Voice: Encourage staff to have a say in workplace problem-solving and decisions. This reaffirms their sense of autonomy and control.
7. Implement Employee Assistance Programs (EAPs) and Peer Support: Strong EAPs offering confidential counselling, along with peer support groups, provide vital mental health resources and opportunities for staff to share experiences.
8. Address Systemic Issues: While challenging, working towards adequate staffing levels and fair pay can substantially reduce ongoing workplace stress.
9. Offer Resilience and Stress Management Training: Providing proactive training can help staff develop techniques to handle stress and strengthen resilience.
2. Foster a Supportive Workplace Culture: Beyond individual efforts, organisations can greatly reduce burnout by creating a culture where staff feel genuinely supported. This involves tackling issues such as feelings of isolation, being undervalued, or bullying.
3. Create Psychologically Safe Spaces: Actively foster environments and opportunities for staff to share their experiences, concerns, and stresses without fear of judgment.
4. Provide Adequate Resources and Training: Ensure staff have the necessary material resources, time, and regular training programs to deliver the best possible care. Opportunities for career advancement also boost job satisfaction and preparedness.
5. Recognise and Appreciate Efforts: Staff who feel their contributions are valued and acknowledged as "making a difference" are less likely to experience burnout. Celebrate their efforts regularly.
6. Empower Staff Voice: Encourage staff to have a say in workplace problem-solving and decisions. This reaffirms their sense of autonomy and control.
7. Implement Employee Assistance Programs (EAPs) and Peer Support: Strong EAPs offering confidential counselling, along with peer support groups, provide vital mental health resources and opportunities for staff to share experiences.
8. Address Systemic Issues: While challenging, working towards adequate staffing levels and fair pay can substantially reduce ongoing workplace stress.
9. Offer Resilience and Stress Management Training: Providing proactive training can help staff develop techniques to handle stress and strengthen resilience.
Conclusion: Investing in Ourselves and Our Future
The challenges of working in aged care in Australia and New Zealand are significant, but so is the dedication and compassion of its workforce. Burnout and compassion fatigue are genuine, impactful issues that can harm both your well-being and the quality of care delivered.
Recognising the signs, understanding the causes, and taking deliberate steps—both individually and as organisations—are essential, not optional. By prioritising self-care, setting boundaries, seeking support, and fostering a genuinely supportive workplace culture, we can build a more resilient and sustainable aged care workforce for the future.
Remember, investing in yourself lets you care for others while looking after your own health and well-being. If you're feeling overwhelmed, don't hesitate to seek professional support or talk to someone you trust. Your well-being matters.
Recognising the signs, understanding the causes, and taking deliberate steps—both individually and as organisations—are essential, not optional. By prioritising self-care, setting boundaries, seeking support, and fostering a genuinely supportive workplace culture, we can build a more resilient and sustainable aged care workforce for the future.
Remember, investing in yourself lets you care for others while looking after your own health and well-being. If you're feeling overwhelmed, don't hesitate to seek professional support or talk to someone you trust. Your well-being matters.
Does this blog resonate with you? Be proactive with your self-care, get plenty of sleep, eat well and exercise. Get help if you need it.
For further reading on other topics, contact the HUB for more topical blogs or further information on what you need to know. EVE will answer a quick question in your own language -easy!
We are on Facebook and LinkedIn. Like us and share our messages with colleagues.
Contact our friendly team if you need help at support@infectionprevention.care
Take advantage of our expertise in IPC. See the HUB for policies, resources and courses relating to this very important subject. Ask EVE for a quick answer to your question.
For further reading on other topics, contact the HUB for more topical blogs or further information on what you need to know. EVE will answer a quick question in your own language -easy!
We are on Facebook and LinkedIn. Like us and share our messages with colleagues.
Contact our friendly team if you need help at support@infectionprevention.care
Take advantage of our expertise in IPC. See the HUB for policies, resources and courses relating to this very important subject. Ask EVE for a quick answer to your question.
Lyndon Forrest
Managing Director | CEO
I am a passionate and visionary leader who has been working in the field of infection prevention and control in aged care for almost 30 years. I am one of the co-founders and the current Managing Director and CEO of Bug Control New Zealand and Australia, the premium provider of infection prevention and control services in aged care. I lead a team that is driven by a common purpose: to help aged care leaders and staff protect their residents from infections and create a healthier future for them.
I am building a business that focuses on our clients and solving their problems. We are focused on building a world-class service in aged care. We focus on being better, not bigger, which means anything we do is for our clients.
I am a passionate and visionary leader who has been working in the field of infection prevention and control in aged care for almost 30 years. I am one of the co-founders and the current Managing Director and CEO of Bug Control New Zealand and Australia, the premium provider of infection prevention and control services in aged care. I lead a team that is driven by a common purpose: to help aged care leaders and staff protect their residents from infections and create a healthier future for them.
I am building a business that focuses on our clients and solving their problems. We are focused on building a world-class service in aged care. We focus on being better, not bigger, which means anything we do is for our clients.
Erica Callaghan
Marketing Manager
Erica Callaghan is a dedicated professional with a rich background in agriculture and nutrient management. Growing up on her family's farm in Mid Canterbury, she developed a deep passion for farming. She currently resides on her partner's arable property in South Canterbury.
In 2017, Erica joined the Farm Sustainability team, focusing on nutrient management and environmental stewardship. In February 2024, she became the Manager of Marketing and Sales at Bug Control New Zealand - Infection Prevention Services, where her passion now includes improving infection prevention outcomes.
Outside of work, Erica loves cooking and traveling, often combining her culinary interests with her explorations in Italy and Vietnam. She enjoys entertaining family and friends and remains actively involved in farm activities, especially during harvest season.
Erica Callaghan is a dedicated professional with a rich background in agriculture and nutrient management. Growing up on her family's farm in Mid Canterbury, she developed a deep passion for farming. She currently resides on her partner's arable property in South Canterbury.
In 2017, Erica joined the Farm Sustainability team, focusing on nutrient management and environmental stewardship. In February 2024, she became the Manager of Marketing and Sales at Bug Control New Zealand - Infection Prevention Services, where her passion now includes improving infection prevention outcomes.
Outside of work, Erica loves cooking and traveling, often combining her culinary interests with her explorations in Italy and Vietnam. She enjoys entertaining family and friends and remains actively involved in farm activities, especially during harvest season.
Toni Sherriff
Clinical Nurse Specialist
Toni is a Registered Nurse with extensive experience in Infection Prevention and Control. Her career began as a kitchen hand and caregiver in Aged Care facilities, followed by earning a Bachelor of Nursing.
Toni has significant experience, having worked in Brisbane’s Infectious Diseases ward before returning home to New Zealand, where she continued her career as a Clinical Nurse Specialist in Infection Prevention and Control within Te Whatu Ora (Health NZ).
Toni brings her expertise and dedication to our team, which is instrumental in providing top-tier infection prevention solutions to our clients.
Toni is a Registered Nurse with extensive experience in Infection Prevention and Control. Her career began as a kitchen hand and caregiver in Aged Care facilities, followed by earning a Bachelor of Nursing.
Toni has significant experience, having worked in Brisbane’s Infectious Diseases ward before returning home to New Zealand, where she continued her career as a Clinical Nurse Specialist in Infection Prevention and Control within Te Whatu Ora (Health NZ).
Toni brings her expertise and dedication to our team, which is instrumental in providing top-tier infection prevention solutions to our clients.
Julie Hadfield
Accounts & Payroll
Julie is experienced in Accounts & Payroll Administration & after a long career in both the Financial & Local Government Sectors, is now working with our team. Julie brings her strong time management & organisational skills to our team, which is important to keep the company running in the background to enable the rest of our team to provide top notch service to all of our clients.
Julie is experienced in Accounts & Payroll Administration & after a long career in both the Financial & Local Government Sectors, is now working with our team. Julie brings her strong time management & organisational skills to our team, which is important to keep the company running in the background to enable the rest of our team to provide top notch service to all of our clients.
Andrea Murray
Content Editor
I attended Otago University in NZ and graduated as a Dental Surgeon. After 40 years in the profession, I retired in 2022. Infection prevention knowledge was part of everyday practice, dealing with sterilisation, hand hygiene, and cleaning.
Before retiring, I began doing some editing and proofreading for Bug Control as I am interested in the subject and in the English language. During the COVID-19 lockdown, I attended the ACIPC course "Introduction to Infection Prevention and Control", which increased my interest in the subject. I now work part-time as the Content Editor for the company.
I attended Otago University in NZ and graduated as a Dental Surgeon. After 40 years in the profession, I retired in 2022. Infection prevention knowledge was part of everyday practice, dealing with sterilisation, hand hygiene, and cleaning.
Before retiring, I began doing some editing and proofreading for Bug Control as I am interested in the subject and in the English language. During the COVID-19 lockdown, I attended the ACIPC course "Introduction to Infection Prevention and Control", which increased my interest in the subject. I now work part-time as the Content Editor for the company.
Personally, I lived in the UK for 10 years. My two children were born in Scotland, and now both are living in Europe, one in Amsterdam, Netherlands, and the other in Edinburgh, Scotland. I live close to Fairlie on the South Island of NZ, a beautiful part of the country, and I love being out of the city.
Princess
Customer Support
Princess began her career as a dedicated Customer Service Representative, honing her communication and problem-solving skills. She later transitioned into a Literary Specialist role, where she developed a keen eye for detail. Her journey then led her to a Sales Specialist position, where she excelled in client relations.
Now, as a Customer Support professional in Infection Prevention Services. Princess focuses on ensuring customer satisfaction, building loyalty, and enhancing the overall customer journey.
Princess began her career as a dedicated Customer Service Representative, honing her communication and problem-solving skills. She later transitioned into a Literary Specialist role, where she developed a keen eye for detail. Her journey then led her to a Sales Specialist position, where she excelled in client relations.
Now, as a Customer Support professional in Infection Prevention Services. Princess focuses on ensuring customer satisfaction, building loyalty, and enhancing the overall customer journey.
Dianne Newey
Senior Infection Prevention and Control Consultant
With over 35 years of experience as a Registered Nurse, I'm now applying all my experience and skills as a Senior Infection Prevention and Control Consultant with Bug Control Infection Prevention Advisory Services.
This is through IP&C education, IP&C environmental audits and reports, IP&C policy and procedure review and development and consultancy on infection prevention and control issues. When I’m not working, I spend time with my family and in my garden, where I grow all my own veggies.
With over 35 years of experience as a Registered Nurse, I'm now applying all my experience and skills as a Senior Infection Prevention and Control Consultant with Bug Control Infection Prevention Advisory Services.
In my role, I promote Infection Prevention and Control, to RACF's and disability support services.
This is through IP&C education, IP&C environmental audits and reports, IP&C policy and procedure review and development and consultancy on infection prevention and control issues. When I’m not working, I spend time with my family and in my garden, where I grow all my own veggies.
Caoimhe (Keva) Stewart
Clinical & Business Operations Manager
Caoimhe is the Manager of Customer Service at Bug Control | Infection Prevention Services, where she ensures that learners have a seamless and supportive experience. With her previous experience as a Registered Nurse in both the UK and Australia, Caoimhe brings a deep understanding of healthcare to her role. Before joining Bug Control IPS Services, she worked in a variety of nursing settings, including Occupational Health, Palliative Care, and Community Nursing, providing her with the ability to empathise with learners and understand the challenges they face.
Caoimhe is the Manager of Customer Service at Bug Control | Infection Prevention Services, where she ensures that learners have a seamless and supportive experience. With her previous experience as a Registered Nurse in both the UK and Australia, Caoimhe brings a deep understanding of healthcare to her role. Before joining Bug Control IPS Services, she worked in a variety of nursing settings, including Occupational Health, Palliative Care, and Community Nursing, providing her with the ability to empathise with learners and understand the challenges they face.
Her move from nursing to customer service was driven by her passion for helping others, not just in clinical settings but also in ensuring that people have access to the resources and support they need. Now, Caoimhe applies her problem-solving skills, attention to detail, and communication expertise to her role, helping to create a positive and effective learning environment for all students.
Outside of work, Caoimhe enjoys travelling, staying active, and catching up with friends on the weekends. Whether in healthcare or customer service, she’s dedicated to making a meaningful difference and supporting people in their personal and professional growth.
Bridgette Mackie
Clinical Nurse Educator
Bridgette is an experienced New Zealand Registered Nurse, qualified Healthcare Auditor, and Healthcare Educator with a strong background in clinical quality, competency assessment, and infection prevention. She has led large-scale OSCE and CAP training programmes for internationally qualified nurses, developed sector-specific educational resources, and coordinated HealthCERT audit preparation in the surgical sector.
Known for her engaging teaching style and genuine passion for supporting learners, Bridgette excels at making complex topics accessible and relevant. She blends operational leadership with a deep commitment to professional development and safe, effective practice.
Bridgette is an experienced New Zealand Registered Nurse, qualified Healthcare Auditor, and Healthcare Educator with a strong background in clinical quality, competency assessment, and infection prevention. She has led large-scale OSCE and CAP training programmes for internationally qualified nurses, developed sector-specific educational resources, and coordinated HealthCERT audit preparation in the surgical sector.
Known for her engaging teaching style and genuine passion for supporting learners, Bridgette excels at making complex topics accessible and relevant. She blends operational leadership with a deep commitment to professional development and safe, effective practice.

